Image Appledene Photographics’
Introduction to the following
The following article raises some interesting points. As a person from the 1950s, at school and university in the 1960s and early 70s , I experienced a cultural shift from the chaos of World War II toward a new hedonism and libertarianism. Pre war and wartime experiences leading to this new world ‘disorder’ are shrouded in official secrecy, on going sentimentality and propaganda as my generation rampaged , hectoring the old championed by a disingenuos big business funding pop culture – and pseudo rebellion.
This social process was , as always, controlled by those with the big money. They decided what to encourage and fund. Feminism was one such phenomenon so encouraged. There was also the hippies and unsex outcome , peace and love responding to the Vietnam war and upper middle class draft dodgers leading the moral war. That war ultimately devolved onto traditional masculinnity and a war on men and their identity.
The workplace and society has been progressively feminised with pseudo equality and a plethora of laws to give women favours and the benefit of the doubt. Boys growing up in a world of absent fathers and girls told they can do and be anything they want is the real source of instability. The author of this article hints at a reality , with religious rather than animal dynamics. He supposed that suicide and other miseries resulting from sex change are caused by it. In my view anyone who wants sex change as a solution to terrible problems is deranged and there should be checks to resolve before surgery.
There is also the matter of asking what the word ‘sex’ means . It has come to mean intercourse rather than the jubilant ‘It’s a boy’ or ‘It’s a girl.’ Now we have a movement to make no decision until the child decides. Religion should have had its day with all this. Religious maniacs of all creed have done much harm to youth with their propensity for delusion and inflicting guilt. Their ranting confuses the issue. We are supposed to be in an age of equality. With so much wealth in so few hands , pull the other one.
There is no doubt that the cosmetic surgery of sex change has many success stories among the higher social classes. But it is poor boys – rarely girls – who overtly declare themselevs the opposite sex. There is no doubt that there is an element of fetishism for some men who enjoy any excuse to wear women’s clothing. Women are masters , or should I say mistresses of disguise. No one dare say that there is an even stronger element of fetishism for women motivating their colossal spending on clothing, shoes , make up, lingerie , perfume and hairdoes. No one dares say , without fear of reprisal, that this clothing is sexual signalling and that they also fetishise men in uniform because they like power. It turns them on.
So I think rather than talk drivel about brains being there to help us make contact with reality, accept the reality that for many, life has always been absolutely horrible and the underclass have even more reason to escape it. Drink , drugs, sex and suicide are increasingly seen as social problems rather the powerful facing up to the centuries of misery they have inflicted on who they see as lower life forms. Now they have patronising out of touch psychiatrists and social workers staffing the likes of Britain’s Tavistock Clinic. In this ‘Slave New World’ some of these people are suggesting their would be big benefits if we were all androgenous. That is a logical progression.
In that case , plastic surgery to change the old fashioned body image shouldn ‘t be a worry. It just becomes a choice of what part you want to play in sexual fantasy relationships now that sex isn’t really about having kids and parenting.
Religious people should face up to reality and stop talking and moralising on the basis of a God that doesn’t exist. Crimes are still being committed in God’s name and his hologram existence has been brought back big time to deceive and blame us. In this world it is not safe being men , but so long as men have daughters things won’t change and the ‘little princess ‘ syndrome will endure. So it is not surprsing that boys want to be princesses too. Freud got so much right.
For more on androgeny , see the site’s ‘Hate Male ‘ page. R,J Cook
BBC Newsnight report on the Tavistock GIDS March 30th 2021
- Post author:Transgender Trend
- Post published:June 20, 2020
- Post category:Health Professionals and Organisations / Media, T.V. & Radio
- Post comments:2 Comments

The report on the Tavistock GIDS, broadcast on Newsnight on Thursday, is the latest installment of a news story that began in 2018.
Towards the end of that year, David Bell, a senior clinician and staff governor at the Tavistock and Portman NHS Trust, produced an internal report containing testimonies from GIDS clinicians, which prompted an internal review. Around the same time a group of parents had submitted a letter to the trust’s board detailing their concerns that young people were being fast-tracked through the service. The Guardian reported on their letter and also on some content they had seen in the Bell report:
“Britain’s only NHS gender identity service for children is reviewing its operations amid claims made by a senior member of staff that it is failing to examine fully the psychological and social reasons behind young people’s desire to change gender.”
In response to the Guardian’s questions about the contents of the report, the Tavistock responded and were quoted:
“The trust is concerned by the tone and manner in which these allegations have been made. They reveal a negative attitude to gender dysphoria and gender identity which does not reflect the views or the approach of the trust.”
Given that the leaked contents of the Bell report suggested serious concerns by clinicians, the review, carried out by the trust’s medical director, Dr Dinesh Sinha, was eagerly awaited – not least by the parents who had written to the trust. In the event, the review accepted some criticisms but failed to reference or address the serious concerns that had been reported by the Guardian.
The Sinha review was followed by an action plan published in March 2019. Paul Jenkins, Chief Executive of Tavistock & Portman NHS Foundation Trust, suggested in the announcement of the plan that concerns had been expressed by only one staff member, from outside GIDS:
“The Trust’s newly appointed Medical Director was commissioned to carry out a Review to explore concerns raised by a member of staff external to the Service.
“The Review did not identify any immediate issues in relation to patient safety or failings in the overall approach taken by the Service in responding to the needs of the young people and families who access its support.”
By then the Bell report had been leaked to the Sunday Times. The contents of the report revealed that the GIDS’ own doctors had “very serious ethical concerns” about children embarking on a life-changing medical pathway without adequate examination or ability to give informed consent.
“It says some children “take up a trans identity as a solution” to “multiple problems such as historic child abuse in the family, bereavement . . . homophobia and a very significant incidence of autism spectrum disorder” after being “coached” online and by trans activist groups.
The true histories of “highly disturbed or complex” child patients were not properly explored by Gids clinicians struggling with “huge and unmanageable caseloads” and afraid of being accused of transphobia if they questioned the “rehearsed” surface presentation. The report says the concerns voiced by staff are shared by Sonia Appleby, who is in charge of safeguarding at the trust.”
The Tavistock responded to the leak with a statement no longer available on their website, but archived here, suggesting this time that some unqualified people had produced an unverified report:
“We are disappointed this unsubstantiated report authored by individuals with no expertise in this field made its way to the Sunday Times and would urge caution about reproducing its content. We do not accept that the vignettes included next to the article are helpful, or representative of the clinical work of the service.”
Marcus Evans, governor and consultant psychotherapist at the Tavistock and Portman trust with three decades’ experience, subsequently resigned, telling the Sunday Times that “the trust had said things that were “not true”, had created a “climate of fear” and was trying to “dismiss or undermine” concerns raised by its own clinicians.””
“I am sad to be ending my proud 34-year association with the trust,” Evans wrote in his resignation letter. “However, I do not have confidence that these serious issues . . . are going to be sufficiently addressed and dealt with in a thorough, thoughtful and balanced way.”
Further critical concerns, this time from former Tavistock clinicians, were reported in the Times in a series of reports from Lucy Bannerman here, here and here, in an issue on April 8th 2019 that also included a comment piece by Dr Carl Heneghan, in which he described the off-label use of drugs for gender dysphoria “an unregulated live experiment on children.”
The Tavistock responded in a statement:
“We strongly reject the claims made in the articles in the Times. The Service always place a young person’s wellbeing at the centre of our work and have a clear position of independence from outside lobby groups on all sides of the debate.”
In July the concerns of the Tavistock staff in London were echoed by a former clinician at the Tavistock Leeds clinic, Kirsty Entwistle, in an open letter to Polly Carmichael.
“I think it is a problem that GIDS clinicians are making decisions that will have a major impact on children and young people’s bodies and on their lives, potentially the rest of their lives, without a robust evidence base. GIDS clinicians tell children and families that puberty blockers/hormone blockers are “fully reversible” but the reality is no one knows what the impacts are on children’s brains so how is it possible to make this claim? It is also a problem that GIDS clinicians are afraid of raising their concerns for fear of being labelled transphobic by colleagues.”
Also in July Newsnight had reported on the Tavistock puberty blockers trial. The report exposed the finding (in some unpublished results) that after a year on blockers a significant increase was found in the first item “I deliberately try to hurt or kill self” in the Youth Self Report questionnaire, a finding by Michael Biggs in his research which was first published by Transgender Trend.
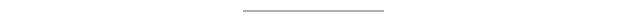
In January this year, Sue Evans, a Psychotherapist, Nurse and ex member of the Tavistock GIDS launched a Judicial Review into the NHS use of puberty blockers, on the grounds that children cannot give informed consent to such experimental treatments. The case has been taken up by Keira Bell, a detransitioned young woman who underwent hormonal treatment at the GIDS, in a joint action with the mother of an autistic girl.
Sue Evans had raised her concerns with the service as early as 2005. An article in the Times ahead of the application for judicial review reported:
“Ms Evans, 62, reported her alarm at the speed of assessment and feared that treatment plans were being influenced by groups such as Mermaids, a transgender advocacy charity.”
In response a Tavistock spokesperson said:
“Our clinical interventions are laid out in nationally-set service specifications. NHS England, monitor our service very closely. The service has a high level of reported satisfaction and was rated good by the Care Quality Commission.”
This is the background and context of the Newsnight report. It was hard to imagine that there could be any new revelations about the Tavistock GIDS by this stage, but the programme revealed “evidence exclusively seen by Newsnight” that suggested even more serious concerns than we had heard before.
Producer Hannah Barnes and reporter Deborah Cohen had seen “well over 100 pages of transcripts, of interviews conducted with staff as part of the review.” Some of the “series of complaints” were familiar from the leaked Bell report, which the Tavistock had attempted to minimise and discredit, but some went further.
“They say decisions about medical treatment were taken too quickly. And they say that some parents appear to prefer that the child was transgender and straight rather than gay – pushing them towards transition.”
“Many children referred to GIDS are extremely distressed and have complex needs. The clinicians we have spoken to say there is often lots to explore before medication should be considered. But they say there is wide variation in practice. It is claimed in the transcripts that many staff are worried and openly discuss their fears.”
“People who raise concerns are seen as troublemakers and difficult. I think it is the case that somehow the organisation works to evacuate people who are not compliant. When I raised concerns I was told that I had to toe the line or I would not progress in my career.”
One clinician was quoted as saying:
“Maybe we are medicating gay children, kids with autism and maybe medicating traumatised children. And if we are, we are doing bad things to these vulnerable kids.”
And another:
“Let us pray that I am wrong. Because if I am not, very many vulnerable children have been very poorly treated and will be left with potentially a lifetime of damage. We’re not talking about little things. The reality is by not doing anything, children are potentially still being medically mismanaged.”
Of even greater concern is the fact that staff reported being discouraged from taking concerns about a child’s welfare to the lead safeguarding officer, or referring cases to social services and seeking advice, and that this came from the Director herself, Polly Carmichael:
“The Tavistock, like other NHS organisations, has a named person that clinicians can turn to to discuss specific safety concerns. That person is Sonia Appleby, but the transcripts allege that staff were discouraged from speaking to her by the director, Polly Carmichael.”
“There was a very clear message from senior management about being really cautious about how we talk to the safeguarding team. Specifically, Sonia Appleby.”
“I have had some consultations with Polly Carmichael about some of the young people I was seeing and some of the concerns I had raised and Polly very directly told me not to go to Sonia to share those concerns.”
We learned that Mrs Appleby could not comment as she had started legal proceedings against the trust last year. The Newsnight report suggests that the most vulnerable children are being put at risk.
“In the transcripts we have seen, clinicians were worried about the impact different kinds of abuse might have on young people trying to resolve questions about their gender identity. These could be seen as safeguarding issues.”
The Newsnight report revealed serious criticisms of individual staff members referring children to a medical pathway after inadequate assessment, in one case within the first hour of meeting:
“NHS England says that young people should be referred for medical treatment, puberty blocking drugs, after a minimum of three sessions. But the review heard from several staff that one member of the leadership, Sarah Davidson, would refer children for treatment after only one or two appointments.”
“I was working with an executive on one case of assessment of a young person and the executive member agrees to refer to this person to the medical pathway within the first hour of meeting him.”
This is in complete contradiction to the “cautious approach to treatment” that the Tavistock claims. According to the GIDS announcement of the Sinha review:
“A comprehensive psychosocial assessment precedes any referral to the endocrine clinic for consideration of physical treatments.”
We also know that the GIDS was alive to the issues of family pressure and acknowledges that often a push to transition comes directly from families:
“…We recognise that there are strongly held views among patients and families and their representatives including those who wish for physical treatment to be offered earlier…”
A serious cause for concern in the Newsnight report is that the complaints were not just about a few rogue clinicians, but extended to the Director of the GIDS herself, Polly Carmichael.
“In some of these cases clinicians thought it would not be appropriate for them to refer for puberty blockers but they would be overruled by GIDS director Polly Carmichael, the transcripts suggest.”
“The young person had clearly told me and my colleague that my mum wants the hormone more than I do and when we took to senior management, Polly Carmichael, she suggested that we refer. Even though this was not clinically indicated.”
“I kept saying to her, are we hurting children? And she did not say no. I kept saying to her, will we get sued and she did not say no. The only solace she gave me is she said it would not be me that would be sued, it would be Tavistock. She was not able to say to me that it is fine, we are not hurting the children.”

No-one from the Tavistock agreed to appear on the programme, instead issuing a statement about the Sinha review:
“We are confident that it fairly addressed the issues raised and strongly refute the allegations put to us by Newsnight”.
The Newsnight report claimed that the transcripts they had seen represent “a sizeable minority of the total number conducted with front line GIDS staff”. The worrying aspect of this is that the majority of staff did not raise these issues, issues relating to a culture of silencing and a management approach which should have been clearly visible to all.
The NHS Gender Identity service seems to view itself as the moderate middle ground between two warring factions of extremists (see this post). The fact is there are two groups, those who operate within the new gender ideology and those who don’t. Within the Tavistock there are clinicians from both sides. Sarah Davidson, for example, was involved with Gendered Intelligence and is a fervent believer in Queer Theory. At one Tavistock conference we attended Davidson urged us all to state our ‘preferred pronouns’ before speaking (nobody did).
Gender ideology demands the sacrifice of established knowledge, training and normal safeguarding protections in service of a belief in an innate gendered soul. Those outside the belief system can see it clearly and have been raising urgent concerns for years. Eventually though, those with conscience will leave the Tavistock, and only the ideologues will remain.
We were told in the report that 40 clinicians had left the GIDS within three years. As one ex-GIDS clinician told us “All the good people are leaving.”
The Care Quality Commission, who rated the GIDS system as ‘good’, has been working with Stonewall since 2012 as part of their Health Champions Scheme. The Tavistock and Portman NHS Trust is also a Stonewall Health Champion. While health institutions remain captured by the ideology of Stonewall, Mermaids and Gendered Intelligence, the homophobic parents consistently referenced by ex-GIDS clinicians can rest easy that their motivation for seeking ‘gender reassignment’ for their children will not be exposed.
“There have been many times when the push to transition has come from families who are uncomfortable with the sexual orientation of their child……some parents express real relief at their child is not gay or lesbian, suggesting being trans is a better outcome for their child”.
Following the Newsnight report there has been no outcry from Stonewall or any other ‘LGBT’ support organisation about this risk to gay and lesbian young people.
The Newsnight report confirmed that the Tavistock GIDS internal review failed to report or adequately address the serious safeguarding concerns reported by staff members and that their complaints extended to management. It is now time for a full investigation into what appear to be serious failings within the Tavistock GIDS current system. An external, independent review is urgently required before more vulnerable children are put at risk.
The crisis at the Tavistock’s child gender clinic Posted March 30th 2021
By Hannah Barnes
BBC NewsnightPublished12 hours ago

In January, England’s only NHS gender clinic for children and young people was rated “inadequate” by the country’s health watchdog – the lowest rating, meaning it is performing badly.
The findings make for sobering reading with inspectors raising “significant concerns” about the way the Gender Identity Development Service (GIDS) works.
Nearly 5,000 children are waiting – sometimes for up to two years – for an appointment, and the management team has been disbanded following the inspection.
Now BBC News has had exclusive sight of an external report written in 2015 which recommended GIDS take drastic action.
It argued the service was “facing a crisis of capacity” to deal with an ever-increasing demand and strikingly it should “take the courageous and realistic action of capping the numbers of referrals immediately”.
With Care Quality Commission inspectors recently confirming many of the risks highlighted still remain, some have expressed concern about why neither GIDS, nor NHS England, which has ultimate responsibility for the service, have done more to help the children and young people it cares for.
By 2015 GIDS, which is part of the Tavistock and Portman NHS Foundation Trust, had been through a period of enormous change.
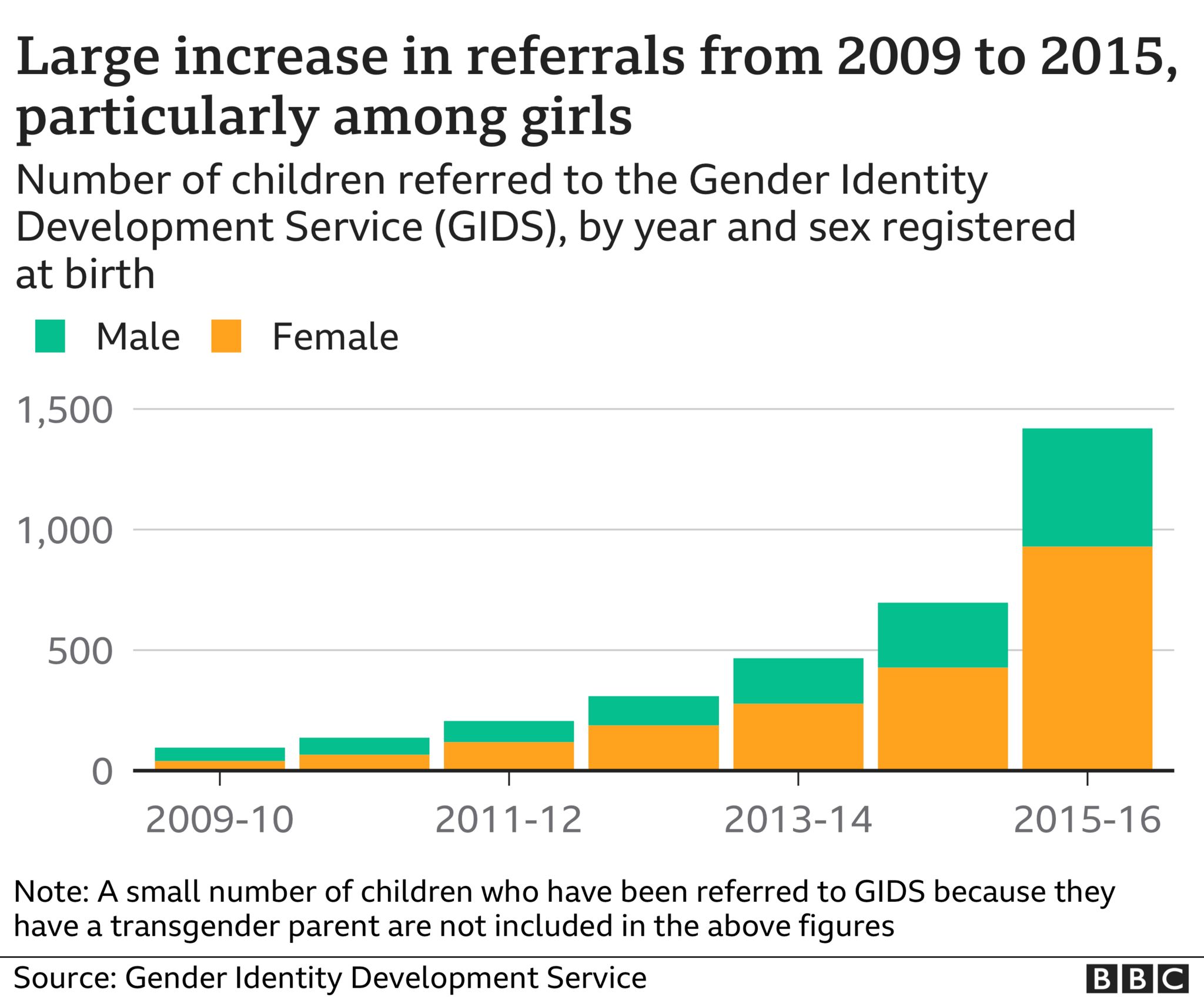
Six years earlier it had become a national service responsible to the central NHS and from that time demand rocketed – increasing 50% per year.
The number of children and young people referred to the service grew from 97 in 2009-10 to 697 in 2014-15.
A second base opened in Leeds in 2011 to help manage demand and ease travel for those living in the north of England.
But accompanying the increase in numbers was a shift in the type of patients being referred.
Since it opened its doors in 1989, around 75% of GIDS’ patients had been boys – natal males to use the language of the service at the time, now referred to as assigned male at birth.
In 2011, girls equalled boys in number for the first time. And by 2015 there had been a reversal in the sex ratio, with girls now outnumbering boys two to one.
What’s more, the nature of the cases appeared to have changed too. Young people often appeared to have complex mental health problems alongside their gender dysphoria – unease caused by a perceived mismatch between biological sex and gender identity.
Many were self-harming; others were struggling with depression, anxiety, bullying or eating disorders. Some suffered traumatic or abusive childhoods.
And finally, medical treatment had become more accessible.
In 2011, a study began to evaluate the impact of administering puberty blockers to younger children. By 2014, when the study had just finished recruiting its final participants, GIDS lowered the age at which young people could be referred for treatment with blockers from 16 to those in the early stages of puberty.
There was no lower age limit as such, but it meant in some instances that children of nine or 10 could now be eligible to be referred for this medical intervention.
By 2015 GIDS was struggling to cope.
Workloads ‘overwhelming’
Official Tavistock Trust board meeting minutes from 2015 support the idea of a service under immense pressure.
In February it’s noted GIDS is becoming more and more stretched, “with activity increasing faster than staffing”.
By June, the minutes are explicit: “The number of complex cases has increased” and it’s clear the environment is challenging.
Several GIDS staff are quoted, and while they enjoy their work one explains how the “demanding caseloads” can feel overwhelming and a “potential threat to the quality and level of work we are able to deliver”.
Another, with a caseload of around 90 young people, says this “can make it difficult to hold clients, their families and the professionals involved in mind”.
“We do not have the resources to offer therapy,” she adds.
Just a month later, the July 2015 minutes record that GIDS director Polly Carmichael acknowledged the service had reached a point where it “would have to say enough” and she was working on how to convey this to NHS England.
The Trust’s then medical director also conceded there was a sense of “escalating risk”, not just from work pressure but also in “the number of safeguarding and risk concerns being brought to him for advice”.
In September, GIDS missed its 18-week waiting time target for the first time.
Against this backdrop, an independent consultant was commissioned by GIDS managers to advise on how the service could adapt to meet growing demand.
One staff member, speaking on condition of anonymity, told the BBC: “We were under a lot of pressure.
“We just couldn’t meet the waiting time target. We hoped by having external consultants they could see what we were doing, because people in management were too close to it. We all were.”
Dr Femi Nzegwu, an international management consultant with over 20 years of experience, was chosen for the task.
Her report on ‘sustainable working’ paints a picture of staff struggling to provide the best care for distressed young people presenting to the service.
“I cannot continue indefinitely with such a high personal caseload with high levels of risk and complexity… without burning out,” one staff member is quoted as saying. “Too busy to stop and reflect on cases and read through current literature which is very risky in this area.
Not all comments are quite so despairing, but there is broad consensus from staff that improvements could and should be made to the way GIDS operates.
It’s important to note that a minority of staff – 19 out of 55 – responded to the questionnaire which formed the basis of Dr Nzegwu’s report.
There’s no way of telling which roles they held – clinical or administrative. At the time GIDS listed its staff number as 34. But the questionnaire was also sent to those at the endocrine clinics that prescribe puberty blocking medication.
‘Cap referrals immediately’
Dr Nzegwu found caseloads were “significant” and continuing to grow, “whilst resources are unlikely to grow to meet expanding needs”.
But perhaps most striking is her primary recommendation that GIDS should “take the courageous and realistic action of capping the number of referrals immediately.”
GIDS should pause. Even if for just a short period, while it reshapes the service.
It’s also recommended that GIDS “agree the criteria for referrals” and on “what the service can realistically deliver” with the resources it has.
Several staff have confirmed to the BBC most GIDS employees were never told of the recommendations.
The report’s findings were shared only during a meeting of the senior team. Serious consideration was given to the recommendation to stop accepting new referrals, the BBC understands. But it was not accepted.
One of those present told the BBC: “The report accurately reflected that we were in some kind of crisis. “The workload was so overwhelming that we didn’t have time to stop, think and ask essential questions
“Had this report been acted on, and indeed even shared internally, GIDS and the Tavistock may have stopped themselves from going down a path which many, least to say some of its patients, may end up regretting,” they said.
It may seem like an extreme option to cap referrals, particularly when there are very distressed children at stake. But, it’s not unheard of. Several Child and Adolescent Mental Health Services (CAMHS) have done this in the past.
Indeed, from the publicly available July 2015 board meeting documents, it appears this option had even been raised as a possibility by GIDS and the wider Tavistock Trust.
The minutes acknowledge referrals criteria might need to be toughened up, noting, “in some cases they might need to refuse a referral if they could not be sure of managing it safely”.
Targets missed
Some suggestions from Dr Nzegwu were acted upon.
Staff were placed into smaller, regional teams and a more obvious career structure was introduced over time.
The service began to assign a ‘complexity’ score to referrals – rating them low, medium or high. But three years later, in June 2018, GIDS director Polly Carmichael conceded, “referrals are received from anyone.”
The new scores did not impact on numbers. Referrals – which could come from GPs, schools, social workers, and even some charities and youth groups – exploded in 2015-16 at their fastest rate yet: more than doubling from the previous year to 1,419.
It’s not surprising, therefore, that having breached its 18-week waiting time target in September 2015, just seven months later waits for young people were approaching a year.
GIDS hasn’t met its target since.
The main change resulting from pressure on the service appears to have been a dramatic increase in the number of GIDS staff – predominantly at a junior level – a suggestion put forward, and funded, by NHS England.
Over the course of the following year the workforce doubled from around 40 to 80.
But this couldn’t solve the fundamental problems GIDS was facing.
The intention was for new junior staff to learn on the job by being paired with senior clinicians. It didn’t work out that way.

In GIDS’ own words: “The rapid growth in the service and associated increase in staff have presented challenges around ensuring adequate training and support for new staff.”
New staff found it “difficult to develop a caseload as quickly as … planned,” Polly Carmichael explained to the Tavistock Trust Board.
“As existing staff already have full caseloads it was difficult for new staff to find experienced co-workers to work with on new cases. The impact of this factor had not been fully appreciated when we recruited the staff,” she said.
But, was it wise to even attempt to staff a service helping a vulnerable patient group with junior staff, with limited clinical experience?
The NHS did not confirm if it had seen the 2015 report. An NHS spokesperson said: “The pressures on the Tavistock relating to rising demand for gender identity services are well known and the NHS has increased investment to respond to the demand for these services.”
Many of the risks highlighted in 2015 remained, and in most cases worsened, by the time the CQC’s inspectors visited GIDS in autumn 2020.
- Caseloads: In 2015 it’s claimed there was an “unspoken expectation” of 100 cases for full-time staff; the CQC says caseloads remain high, “stressful and difficult to manage”
- Patient assessments: Questions are asked about uniformity and minimum standards of report writing in 2015; the CQC describes assessments as “unstructured, inconsistent and poorly recorded”
- Risk: Staff raised concerns about the level of risk in the service in 2015; the CQC found GIDS did “not always manage risk well” both for patients in the service and those on the waiting list
There are now over 4,600 young people on that GIDS waiting list, with some waiting over two years for their first appointment. A far cry from the 18-weeks when Dr Nzegwu made her recommendations.
Concerns raised again
Dr David Bell, a highly respected psychiatrist at the Tavistock Trust, and one-time staff governor believes had the Tavistock responded in an “appropriate manner” in 2015 “further harm to children and young people might have been avoided”.
GIDS staff raised their concerns to him again in 2018 after they felt conversations with GIDS managers and other senior Tavistock Trust figures had made no impact.
He presented those concerns to the Trust’s board in August 2018, concluding that GIDS was “not fit for purpose” and “children’s needs are being met in a woeful inadequate manner”.
When he saw Dr Nzegwu’s 2015 report a year later, Dr Bell, who recently retired, said he was “very surprised to see a number of the concerns that were raised in my report, were either directly mentioned in this report or were related to them.
“There is of course a straight line from the concerns raised in this report and in my report to those in the report of the CQC.”
The Tavistock Trust’s medical director conducted a review of GIDS in 2019 in response to Dr Bell’s findings, and while the need for improvements was accepted, the Trust said, “it did not identify any immediate issues in relation to patient safety”.
When asked by BBC News, the Tavistock did not confirm whether anyone in the wider Trust – outside of GIDS – had seen the 2015 report, nor answer why its recommendations appeared to not have been acted upon and whether this could have impacted the current service.
In a statement, a spokesperson said: “GIDS is and has always been alive to issues relating to capacity in the face of rapidly rising referrals.”
“This has been the subject of ongoing discussions with NHS England,” they added.
“We are working closely with both the CQC and NHS England to work out how we can best manage demand for our service and those patients waiting to be seen. An action plan is in place.”
Limited support from other services
While advice from 2015 doesn’t appear to have been acted upon, it seems there was also limited support for GIDS patients from other services.
The surge in demand for GIDS’ expertise coincided with increased pressure on CAMHS.
“Some of the young people we see in the service experience difficulties which may or may not be related to gender dysphoria,” a Tavistock spokesperson told the BBC in October 2020.
For it to work at its best, GIDS relies on being able to work “closely with local CAMHS to support ongoing difficulties”.
“It is important to recognise not all co-occurring difficulties will be resolved by accessing specialist psychosocial exploration of gender identity and related issues,” they said.
There are also questions for NHS England. How was it that as reports questioning both GIDS’ model and, in later years, its ability to offer the best care possible to every single patient surfaced, it didn’t step in?
“An objective observer could see essential restructuring was needed to ensure a safe service for staff and patients as far back as 2015,” the GIDS staff member said.
Dr David Bell goes further.
“It is, to put it mildly, surprising that given the degree of mismanagement and serious neglect they [NHS England] have not intervened.”
The NHS announced an independent review into gender identity services for children and young people in September 2020, which GIDS supports.
That review, led by Dr Hilary Cass will “help ensure any child or young person, who may be dealing with a complexity of issues around their gender identity, gets access to the best possible support and expertise care,” an NHS spokesperson said.
Much now rests on the Cass review, which may yet take some time to complete.

Sex Reassignment Doesn’t Work. Here Is the Evidence. Posted February 8th 2021
Mar 9th, 2018 15 min read

Ryan T. Anderson, Ph.D.@RyanTAnd
Former Senior Research Fellow Ryan T. Anderson, Ph.D., researched and wrote about marriage, bioethics, religious liberty and political philosophy.

Key Takeaways
McHugh points to the reality that because sex change is physically impossible, it frequently does not provide the long-term wholeness and happiness that people seek.
Unfortunately, many professionals now view health care—including mental health care—primarily as a means of fulfilling patients’ desires, whatever those are.
Our brains and senses are designed to bring us into contact with reality, connecting us with the outside world and with the reality of ourselves. Copied
Sex “reassignment” doesn’t work. It’s impossible to “reassign” someone’s sex physically, and attempting to do so doesn’t produce good outcomes psychosocially.
As I demonstrate in my book, “When Harry Became Sally: Responding to the Transgender Moment,” the medical evidence suggests that sex reassignment does not adequately address the psychosocial difficulties faced by people who identify as transgender. Even when the procedures are successful technically and cosmetically, and even in cultures that are relatively “trans-friendly,” transitioners still face poor outcomes.
Dr. Paul McHugh, the university distinguished service professor of psychiatry at the Johns Hopkins University School of Medicine, explains:
Transgendered men do not become women, nor do transgendered women become men. All (including Bruce Jenner) become feminized men or masculinized women, counterfeits or impersonators of the sex with which they ‘identify.’ In that lies their problematic future.
When ‘the tumult and shouting dies,’ it proves not easy nor wise to live in a counterfeit sexual garb. The most thorough follow-up of sex-reassigned people—extending over 30 years and conducted in Sweden, where the culture is strongly supportive of the transgendered—documents their lifelong mental unrest. Ten to 15 years after surgical reassignment, the suicide rate of those who had undergone sex-reassignment surgery rose to 20 times that of comparable peers.
McHugh points to the reality that because sex change is physically impossible, it frequently does not provide the long-term wholeness and happiness that people seek.
Indeed, the best scientific research supports McHugh’s caution and concern.
Here’s how The Guardian summarized the results of a review of “more than 100 follow-up studies of post-operative transsexuals” by Birmingham University’s Aggressive Research Intelligence Facility:
[The Aggressive Research Intelligence Facility], which conducts reviews of health care treatments for the [National Health Service], concludes that none of the studies provides conclusive evidence that gender reassignment is beneficial for patients. It found that most research was poorly designed, which skewed the results in favor of physically changing sex. There was no evaluation of whether other treatments, such as long-term counseling, might help transsexuals, or whether their gender confusion might lessen over time.
“There is huge uncertainty over whether changing someone’s sex is a good or a bad thing,” said Chris Hyde, the director of the facility. Even if doctors are careful to perform these procedures only on “appropriate patients,” Hyde continued, “there’s still a large number of people who have the surgery but remain traumatized—often to the point of committing suicide.”
Of particular concern are the people these studies “lost track of.” As The Guardian noted, “the results of many gender reassignment studies are unsound because researchers lost track of more than half of the participants.” Indeed, “Dr. Hyde said the high drop-out rate could reflect high levels of dissatisfaction or even suicide among post-operative transsexuals.”
Hyde concluded: “The bottom line is that although it’s clear that some people do well with gender reassignment surgery, the available research does little to reassure about how many patients do badly and, if so, how badly.”
The facility conducted its review back in 2004, so perhaps things have changed in the past decade?
Not so. In 2014, a new review of the scientific literature was done by Hayes, Inc., a research and consulting firm that evaluates the safety and health outcomes of medical technologies. Hayes found that the evidence on long-term results of sex reassignment was too sparse to support meaningful conclusions and gave these studies its lowest rating for quality:
Statistically significant improvements have not been consistently demonstrated by multiple studies for most outcomes. … Evidence regarding quality of life and function in male-to-female adults was very sparse. Evidence for less comprehensive measures of well-being in adult recipients of cross-sex hormone therapy was directly applicable to [gender dysphoric] patients but was sparse and/or conflicting. The study designs do not permit conclusions of causality and studies generally had weaknesses associated with study execution as well. There are potentially long-term safety risks associated with hormone therapy but none have been proven or conclusively ruled out.
The Obama administration came to similar conclusions. In 2016, the Centers for Medicare and Medicaid Services revisited the question of whether sex reassignment surgery would have to be covered by Medicare plans. Despite receiving a request that its coverage be mandated, it refused, on the ground that we lack evidence that it benefits patients.
Here’s how the June 2016 “Proposed Decision Memo for Gender Dysphoria and Gender Reassignment Surgery” put it:
Based on a thorough review of the clinical evidence available at this time, there is not enough evidence to determine whether gender reassignment surgery improves health outcomes for Medicare beneficiaries with gender dysphoria. There were conflicting (inconsistent) study results—of the best designed studies, some reported benefits while others reported harms. The quality and strength of evidence were low due to the mostly observational study designs with no comparison groups, potential confounding, and small sample sizes. Many studies that reported positive outcomes were exploratory type studies (case-series and case-control) with no confirmatory follow-up.
The final August 2016 memo was even more blunt. It pointed out:
Overall, the quality and strength of evidence were low due to mostly observational study designs with no comparison groups, subjective endpoints, potential confounding (a situation where the association between the intervention and outcome is influenced by another factor such as a co-intervention), small sample sizes, lack of validated assessment tools, and considerable lost to follow-up.
That “lost to follow-up,” remember, could be pointing to people who committed suicide.
And when it comes to the best studies, there is no evidence of “clinically significant changes” after sex reassignment:
The majority of studies were non-longitudinal, exploratory type studies (i.e., in a preliminary state of investigation or hypothesis generating), or did not include concurrent controls or testing prior to and after surgery. Several reported positive results but the potential issues noted above reduced strength and confidence. After careful assessment, we identified six studies that could provide useful information. Of these, the four best designed and conducted studies that assessed quality of life before and after surgery using validated (albeit non-specific) psychometric studies did not demonstrate clinically significant changes or differences in psychometric test results after [gender reassignment surgery].
In a discussion of the largest and most robust study—the study from Sweden that McHugh mentioned in the quote above—the Obama Centers for Medicare and Medicaid Services pointed out the 19-times-greater likelihood for death by suicide, and a host of other poor outcomes:
The study identified increased mortality and psychiatric hospitalization compared to the matched controls. The mortality was primarily due to completed suicides (19.1-fold greater than in control Swedes), but death due to neoplasm and cardiovascular disease was increased 2 to 2.5 times as well. We note, mortality from this patient population did not become apparent until after 10 years. The risk for psychiatric hospitalization was 2.8 times greater than in controls even after adjustment for prior psychiatric disease (18 percent). The risk for attempted suicide was greater in male-to-female patients regardless of the gender of the control. Further, we cannot exclude therapeutic interventions as a cause of the observed excess morbidity and mortality. The study, however, was not constructed to assess the impact of gender reassignment surgery per se.
These results are tragic. And they directly contradict the most popular media narratives, as well as many of the snapshot studies that do not track people over time. As the Obama Centers for Medicare and Medicaid pointed out, “mortality from this patient population did not become apparent until after 10 years.”
So when the media tout studies that only track outcomes for a few years, and claim that reassignment is a stunning success, there are good grounds for skepticism.
As I explain in my book, these outcomes should be enough to stop the headlong rush into sex reassignment procedures. They should prompt us to develop better therapies for helping people who struggle with their gender identity.
And none of this even begins to address the radical, entirely experimental therapies that are being directed at the bodies of children to transition them.
Sex Change Is Physically Impossible
We’ve seen some of the evidence that sex reassignment doesn’t produce good outcomes psychosocially. And as McHugh suggested above, part of the reason why is because sex change is impossible and “it proves not easy nor wise to live in a counterfeit sexual garb.”
But what is the basis for the conclusion that sex change is impossible?
Contrary to the claims of activists, sex isn’t “assigned” at birth—and that’s why it can’t be “reassigned.” As I explain in “When Harry Became Sally,” sex is a bodily reality that can be recognized well before birth with ultrasound imaging. The sex of an organism is defined and identified by the way in which it (he or she) is organized for sexual reproduction.
This is just one manifestation of the fact that natural organization is “the defining feature of an organism,” as neuroscientist Maureen Condic and her philosopher brother Samuel Condic explain. In organisms, “the various parts … are organized to cooperatively interact for the welfare of the entity as a whole. Organisms can exist at various levels, from microscopic single cells to sperm whales weighing many tons, yet they are all characterized by the integrated function of parts for the sake of the whole.”
Male and female organisms have different parts that are functionally integrated for the sake of their whole, and for the sake of a larger whole—their sexual union and reproduction. So an organism’s sex—as male or female—is identified by its organization for sexually reproductive acts. Sex as a status—male or female—is a recognition of the organization of a body that can engage in sex as an act.
That organization isn’t just the best way to figure out which sex you are. It’s the only way to make sense of the concepts of male and female at all. What else could “maleness” or “femaleness” even refer to, if not your basic physical capacity for one of two functions in sexual reproduction?
The conceptual distinction between male and female based on reproductive organization provides the only coherent way to classify the two sexes. Apart from that, all we have are stereotypes.
This shouldn’t be controversial. Sex is understood this way across sexually reproducing species. No one finds it particularly difficult—let alone controversial—to identify male and female members of the bovine species or the canine species. Farmers and breeders rely on this easy distinction for their livelihoods. It’s only recently, and only with respect to the human species, that the very concept of sex has become controversial.
And yet, in an expert declaration to a federal district court in North Carolina concerning H.B. 2 (a state law governing access to sex-specific restrooms), Dr. Deanna Adkins stated, “From a medical perspective, the appropriate determinant of sex is gender identity.” Adkins is a professor at Duke University School of Medicine and the director of the Duke Center for Child and Adolescent Gender Care (which opened in 2015).
Adkins argues that gender identity is not only the preferred basis for determining sex, but “the only medically supported determinant of sex.” Every other method is bad science, she claims: “It is counter to medical science to use chromosomes, hormones, internal reproductive organs, external genitalia, or secondary sex characteristics to override gender identity for purposes of classifying someone as male or female.”
In her sworn declaration to the federal court, Adkins called the standard account of sex—an organism’s sexual organization—“an extremely outdated view of biological sex.”
Dr. Lawrence Mayer responded in his rebuttal declaration: “This statement is stunning. I have searched dozens of references in biology, medicine and genetics—even Wiki!—and can find no alternative scientific definition. In fact, the only references to a more fluid definition of biological sex are in the social policy literature.”
Just so. Mayer is a scholar in residence in the Department of Psychiatry at the Johns Hopkins University School of Medicine and a professor of statistics and biostatistics at Arizona State University.
Modern science shows that our sexual organization begins with our DNA and development in the womb, and that sex differences manifest themselves in many bodily systems and organs, all the way down to the molecular level. In other words, our physical organization for one of two functions in reproduction shapes us organically, from the beginning of life, at every level of our being.
Cosmetic surgery and cross-sex hormones can’t change us into the opposite sex. They can affect appearances. They can stunt or damage some outward expressions of our reproductive organization. But they can’t transform it. They can’t turn us from one sex into the other.
“Scientifically speaking, transgender men are not biological men and transgender women are not biological women. The claims to the contrary are not supported by a scintilla of scientific evidence,” explains Mayer.
Or, as Princeton philosopher Robert P. George put it, “Changing sexes is a metaphysical impossibility because it is a biological impossibility.”
The Purpose of Medicine, Emotions, and the Mind
Behind the debates over therapies for people with gender dysphoria are two related questions: How do we define mental health and human flourishing? And what is the purpose of medicine, particularly psychiatry?
Those general questions encompass more specific ones: If a man has an internal sense that he is a woman, is that just a variety of normal human functioning, or is it a psychopathology? Should we be concerned about the disconnection between feeling and reality, or only about the emotional distress or functional difficulties it may cause?
What is the best way to help people with gender dysphoria manage their symptoms: by accepting their insistence that they are the opposite sex and supporting a surgical transition, or by encouraging them to recognize that their feelings are out of line with reality and learn how to identify with their bodies?
All of these questions require philosophical analysis and worldview judgments about what “normal human functioning” looks like and what the purpose of medicine is.
Settling the debates over the proper response to gender dysphoria requires more than scientific and medical evidence. Medical science alone cannot tell us what the purposeof medicine is.
Science cannot answer questions about meaning or purpose in a moral sense. It can tell us about the function of this or that bodily system, but it can’t tell us what to do with that knowledge. It cannot tell us how human beings ought to act. Those are philosophical questions, as I explain in “When Harry Became Sally.”
While medical science does not answer philosophical questions, every medical practitioner has a philosophical worldview, explicit or not. Some doctors may regard feelings and beliefs that are disconnected from reality as a part of normal human functioning and not a source of concern unless they cause distress. Other doctors will regard those feelings and beliefs as dysfunctional in themselves, even if the patient does not find them distressing, because they indicate a defect in mental processes.
But the assumptions made by this or that psychiatrist for purposes of diagnosis and treatment cannot settle the philosophicalquestions: Is it good or bad or neutral to harbor feelings and beliefs that are at odds with reality? Should we accept them as the last word, or try to understand their causes and correct them, or at least mitigate their effects?
While the current findings of medical science, as shown above, reveal poor psychosocial outcomes for people who have had sex reassignment therapies, that conclusion should not be where we stop. We must also look deeper for philosophical wisdom, starting with some basic truths about human well-being and healthy functioning.
We should begin by recognizing that sex reassignment is physically impossible. Our minds and senses function properly when they reveal reality to us and lead us to knowledge of truth. And we flourish as human beings when we embrace the truth and live in accordance with it. A person might find some emotional relief in embracing a falsehood, but doing so would not make him or her objectively better off. Living by a falsehood keeps us from flourishing fully, whether or not it also causes distress.
This philosophical view of human well-being is the foundation of a sound medical practice. Dr. Michelle Cretella, the president of the American College of Pediatricians—a group of doctors who formed their own professional guild in response to the politicization of the American Academy of Pediatrics—emphasizes that mental health care should be guided by norms grounded in reality, including the reality of the bodily self.
“The norm for human development is for one’s thoughts to align with physical reality, and for one’s gender identity to align with one’s biologic sex,” she says. For human beings to flourish, they need to feel comfortable in their own bodies, readily identify with their sex, and believe that they are who they actually are. For children especially, normal development and functioning require accepting their physical being and understanding their embodied selves as male or female.
Unfortunately, many professionals now view health care—including mental health care—primarily as a means of fulfilling patients’ desires, whatever those are. In the words of Leon Kass, a professor emeritus at the University of Chicago, today a doctor is often seen as nothing more than “a highly competent hired syringe”:
The implicit (and sometimes explicit) model of the doctor-patient relationship is one of contract: the physician—a highly competent hired syringe, as it were—sells his services on demand, restrained only by the law (though he is free to refuse his services if the patient is unwilling or unable to meet his fee). Here’s the deal: for the patient, autonomy and service; for the doctor, money, graced by the pleasure of giving the patient what he wants. If a patient wants to fix her nose or change his gender, determine the sex of unborn children, or take euphoriant drugs just for kicks, the physician can and will go to work—provided that the price is right and that the contract is explicit about what happens if the customer isn’t satisfied.
This modern vision of medicine and medical professionals gets it wrong, says Kass. Professionals ought to profess their devotion to the purposes and ideals they serve. Teachers should be devoted to learning, lawyers to justice, clergy to things divine, and physicians to “healing the sick, looking up to health and wholeness.” Healing is “the central core of medicine,” Kass writes—“to heal, to make whole, is the doctor’s primary business.”
To provide the best possible care, serving the patient’s medical interests requires an understanding of human wholeness and well-being. Mental health care must be guided by a sound concept of human flourishing. The minimal standard of care should begin with a standard of normality. Cretella explains how this standard applies to mental health:
One of the chief functions of the brain is to perceive physical reality. Thoughts that are in accordance with physical reality are normal. Thoughts that deviate from physical reality are abnormal—as well as potentially harmful to the individual or to others. This is true whether or not the individual who possesses the abnormal thoughts feels distress.
Our brains and senses are designed to bring us into contact with reality, connecting us with the outside world and with the reality of ourselves. Thoughts that disguise or distort reality are misguided—and can cause harm. In “When Harry Became Sally,” I argue that we need to do a better job of helping people who face these struggles.
This piece originally appeared in The Daily Signal More on This Issue
British Police Institutionally Corrupt in an Institutionally Corrupt Police State December 18th 2020
robertajane.cook <robertajane.cook@btinternet.com>To: Joseph Hilton J.Hilton@oakwoodsolicitors.co.uk; Amanda Hawke AHawke@tavi-port.nhs.uk; gmc@gmc-uk.org; nordenhouseadmin@nhs.net;18/12/20 19:284Correction was necessary to my previous message, for legal reasons.

Thank you very much for your reply. I do not accept the statute of limitation argument because the matter is ongoing , with neither GIC or GMC explaining themselves. Also, if one takes February 2018, as the start point, then there are still 2 plus months to play with inside the Statute of Limitations.. There was even more time from the date of my original message to yourselves. Thus you are giving me incorrect legal opinion rather than your true reasons for refusing me representation – and are thus, either liars or incompetent.
You were informed that the malicious NHS PPD diagnosis was in May 2018, which gives even more leeway for legal action.Three years is three years, not two years and a bit. However, since the GIC have yet to explain my current status with them , why I have not been formally discharged and why,, method of diagnosing PPD. lack explanation and treatment other than to say that seeing all of the records would upset me, then we have an ongoing legal and even criminal situation – for which the Statute of Limitations countdown has not yet started. How could I possibly know a start date for NHS malpractice until I have received answers to key questions that all parties so far refuse to answer ?
In a nutshell, the police and their over 13 years of malicious misconduct – including hiding evidence and lies about domestic violence, alcoholism, and God knows what else, passed to my GP who meanwhile approved my medical and mental fitness to drive heavy trucks for many years – led to the cutting off of my GIC treatment at a crucial stage, unless I my accepted my paranoia and anti psychoric drugs. That is the essence of my claim. Refusal to recognise this and the consequences means the involved public services, notably police and NHS, are committing ongoing abuse and misconduct, meaning the Statute of Limitations has not even started.
Anyone with a claim to psychiatric or psychological qulaification, would know that the only way to verify my thoughts being delusional would be to test the evidence for or against what I am saying. They would also know why innocent people will never admit guilt, preferring death. It is the same psychological process preventing rape victims from backing off – just so you know, my opinions are based on qualifications and experience, not delusions.
This was because the police have continued their vile and despicable behaviour because they hoped, in the absence of jailing me, to label me paranoid and delusional . Their self interested perjury, misconduct in public office and conspiracy to pervert the course of justice must not be questioned because the public always trust and believe them.. They also brought malicious allegations of prostitution and my son running a brothel.They made sure these vile lies were passed to my GP and Norden House who passed them to GIC and Whiteleaf Pyschiatric Facility. Hence their conclusion that I am more likely to die by misadventure than suicide – I am 70, but curiously death caused by a combination of the stress they have caused, along with my old age, was not mentioned on the Whiteleaf report.
The police lost the prostitution and consequent verbal abuse cases too – though no doubt never informed my so called NHS carers who would have pased these lies to lawyers on both sides. I don’t expect an honest answer from you. British law. Judges and lawyers on both sides, are about money and status – not justice.
There is a prima facie case that the NHS willingly allowed their judgement to be guided by corrupt self interested police. I didn’t spell that out in initial correspondence because I needed you to do what you have done – come up with a pathetic patronising piece of pseudo legalise at the behest of aforementioned parties, thus exposing the police even more so.. After all, the police never lie or abuse anyone who isn’t black (sic ) , do they ?)
I expected your inquiries to lead you, via Norden House, to police criminal lies ( about domestic violence that never happened, demonstrably untrue events that were never investigated because of corrupt senior police officers – including my ex brother in law who stood to gain from my divorce ). with the inevitable proviso that I must not be told. This message, witrh yours will now be posted on my website, About R.J Cook page, together with adverse comments on your competency and honesty. The site is www.robertcookofnorthbucks.com . Your response will be relevant to a forthcoming Crown Court trial.. Police and their associates read my site daily. The police had their chance to leave me alone, but chose to interfere with my medical care with devastating effects, added to all of their other harm done.
Yours Sincerely R.J Cook
—— Original Message ——
From: “Joseph Hilton” <J.Hilton@oakwoodsolicitors.co.uk>
To: “robertajane.cook@btinternet.com” <robertajane.cook@btinternet.com>
Sent: Friday, 4 Dec, 20 At 11:36
Subject: Your Legal Enquiry with Oakwood Solicitors
Dear Ms Cook,
Re: Your Recent Clinical Negligence Enquiry
Thank you for your recent enquiry to Oakwood Solicitors Limited.
I have had the chance to review the information that you have provided. Unfortunately we are unable to assist you on this occasion due to the fact that Limitation is an issue, that being we have insufficient time to investigate. I would consider from the facts that you have provided e have less than a year to investigate the claim. As a result, we are unable to take the case on under a Conditional Fee Agreement (a No Win, No Fee Agreement).
If there is a material change in the evidence that you have provided to us, please do not hesitate to get in touch once again and we can review it for you.
We would recommend that you seek urgent legal advice if you are determined to find legal representation on a Conditional Fee basis. Please be aware that your claim will be subject to a three year limitation period .
This means that Court proceedings must be commenced within the Courts of England and Wales within three years of either the date the negligent act occurred or the date a reasonable person ought to have been aware that negligence had occurred. In cases involving a deceased this three year period commences from the date of death. This limitation period is extended in cases involving minors and in such instances Court proceedings must commence by their 21st Birthday. Claims brought after the expiration of the limitation period will be statute barred and only heard with the express permission of the Courts.
You can use the Law Society’s Find A Solicitor website to find a firm which provides the required legal services (https://www.lawsociety.org.uk) or by calling 020 7320 5650 (Monday to Friday from 09:00 to 17:00, charged at local call rates).
We are sorry that we have been unable to assist you on this occasion. We sincerely hope that you are able to obtain a positive outcome to your claim.
Whilst we cannot assist you on a No Win,No Fee Basis in relation to this particular matter, we would like to inform you that Oakwood Solicitors are specialists in a number of other legal areas. Please note some of the other services that may be of interest to you:-
- Road Traffic Accidents – road traffic accidents that were not your fault (this may include accidents in motor vehicles as a driver or passenger, motor bikes, as a pedestrian, on the bus or on a push bike).
- Employment Liability claims – accidents at work that were due to the negligence of your employers such as manual handling, defective equipment or lack of protective equipment.
- Employment – All kinds of claims arising from employment. We cover the full range of claims and can advise on everything from unfair dismissal to complex discrimination issues.
- Public Liability claims – slips and trips on the public high way as well as in public areas such as shops and supermarkets.
- Industrial Deafness – if your hearing is worse than it should be for someone of your age and you worked at a noisy workplace.
- Payment Protection Insurance – if you have you been sold a PPI policy alongside a loan against your wishes or that you did not know about then you could be entitled to claim.
- CICA Claims – if you have been a victim of a physical or mental injury due to a violent crime and you have cooperated with the police at all times then you can make a Criminal Injuries claim.
- Stress at work – We are experts in recovering damages for claims arising out of stress at work whether it be caused by bullying, harassment or an excessive workload.
- Product liability – injuries resulting from defective products or goods.
- Breach of Insurance Claims – has your insurer refused to satisfy your claim under an insurance policy? We are experts in recovering damages against insurers in respect of the insurer’s breach of contract.
- Sports Injuries – Have you suffered an injury as a result of a sporting accident? We are experts in thefield of sports injury compensation.
- Property – residential sales and purchases, remortgages and transfers of equity. Commercial property sales and purchases, leases and development.
- Wills and Probate – Have you got your affairs in order? When was the last time your Will was updated? What will happen if you loose mental capacity who will take care of things for you? We are experts in the field in Wills and probate and offer impartial advice and services to ensure that your wishes are fulfilled.
If you require advice on any of the above then please do not hesitate to call us on 0113 200 9720 and we will ask one of our dedicated staff to give you free advice on your potential claim.
Once again, thank you for contacting Oakwood Solicitors about this legal enquiry.
Kind regards,
Today I learned that malicious unfounded criminal allegations by certain parties, including stalking, domestic violence and mental illness have thwarted my son and I from being able to register as a Private Limited Company. We cannot work as professionals, let property or become company directors due to police lies and corruption.
Added to the illegal unexplained PNC Criminal Marker created by corrupt Chief Constable Paul West of West Mercia Police, for reasons I cannot disclose with court action pending, that, Marker and malicious so called soft intelligence created by West Mercia Police and backed up by Thames Valley, dating as far as I know from October 4th/5th 2008 – maybe earlier- for stalking and violence threats when I was hundreds of miles away, has had life destroying effects on mine and my son’s lives.
So as a result, it transpires that my address has been referred presumably due to this police marker on the house, according to sources – all of this with allegations and corrupt diagnosis that I have a paranoid personality disorder, am deluded and with abnormal psychology, unable to get on with other people.

For the last 13 years, two police forces have refused to investigate these malicious allegations, or my counter allegations, lying to CPS , my lawyers, press and courts about investigations and spending thousands to get me jailed – lying to my lawyers via the CPS. they have conspired to protect the police in misconduct, perjury and conspiracy to pervert the course of justice, which is why they lost their last two malicious prosecutions against me, again conspiring to pervert the course of justice. I know why.
An official mental health report has concluded that I compulsively take risks in life, have paranoid delusions and am more likely to die by misadventure than suicide. I am 70 plus, but they never mention old age.
Police roped my obsequious doctors in to back up their monitoring exercise – also accusing me of alcoholism even though my GP signed off on my HGV medicals that I am not alcoholic or mentally ill.
With my long shifts, I had routine drug and alcohol tests. Because of the malicious police marker dating from October 9th 2008, I was routinely and dangerously chased by marked and unmarked police cars – including into work, presumably to get me sacked-, searched and never found to be in possession of drugs, weapons or ‘in drink.; Malice from certain parties is obvious.
During my last 18 hour confinement in a dirty cold dark police cell, I felt there was no choice but suicide – found chocking myself with my tee shirt and semi conscious, around 10 pm, under a blanket after about 10 minutes of effort, trapping the shirt under my neck so that as conciousness faded, the shirt tightened under my weight. I would certainly do it again in the absence of an honest independent investigation and/or trial. Life as I and my eldest son have had it for nearly 14 years isn’t worth it.
I was transferred at 1 a.m ( 0100 hours ) to a mental hospital for another 11 hours before two doctors and a senior female mental health specialist judged me sane. That doesn’t mean I will not eventually kill myself because the police and CPS, along with local and mainstream media have made my life unbearable, also exposing me to abuse in the street, vandalism, unemployment, professional ruin and poverty.
Covid has wrecked my finances totally and homelessness is imminent unless I kill myself. I am telling the truth . Life like this just isn’t worth it. My son agrees.
I presume they got the misadventure idea from interested parties and work on my confiscated computers , a draft novel about a transsexual who wants to be murdered to banish ‘The Woman Within’ – derivative of Kafka’s ‘Metamorphosis.’. A novel based on my domestic horrors, ‘Little Terrors’ was published in 2003 – along with 5 other of my books.
Free thinking and expression is not allowed in Britain , especially for one who used to be close to police circles. Only females, especially feminists are allowed to write about and question the conventional wisdom of gender and sexuality in the current social climate. That is life in a police state.
R.J Cook

The following will only make sense if read in conjuction with material on the ‘About R.J Cook’ page. This letter has been sent to a lawyer for legal opinion. The matter is complicated by ongoing police intrusion into my life as they have an ongoing cover up of their criminal misconduct toward me. The missing and key dynamic here is the police. They have lied to CPS, my expensive lawyers, press and courts, as well as the NHS concerning my case.
Labelling me mentally ill and having me sectioned is the next best thing to having me jailed. There is an old saying about the police when it comes to framing innocents of any colour. ‘They never give up.’ Of course that is no excuse for the vested interests of the NHS and the gender reassignment industry.
To those who would argue that I have set them up for journalistic purposes, winding up the corrupt police in the process for purposes of disclosures, I would answer, ‘It was not my job to make a diagnosis about my gender identity.’
One of the most significant memories I have from early consultations was being asked what part of my body I disliked the most, and was I wearing female underwear. To the first question, I replied that I knew a 70 plus man who had been paralysed since being run over in 1952, so was glad everything was still working. To the second question, I replied ‘No’.
Through the whole process, I was never asked why I didn’t like being a man, or why I left it so long to do something about it ? Radical Trans Exclusionary Radical Feminists ( TERF ) have a self centred egotistical attitude to sex change clinics like Tavistock. Feminists have the weird arrogance of all religious fanatics. a sense of owning the truth, deciding what is right.
They accept no resonsibility for their increasingly male mimicry, strident and ridiculing attitude to me creating incompetent one parent families and deluded little boys copying mummy, looking for the safety and approval they think comes from wearing female clothes, shoes and make up. Meantime, the weird and dubuous behavior of the likes of Tavistock are never questioned. This is because, as sacking the Eton Master attests, is because feminism must never be challenged.
Thanks for getting back to me and I apologise for the delay in replying. I have given an outline of my situation below, as briefly as possible. More details and documents are available, if you feel you can help and proceed. My health is getting worse as a result of all that has happened to me. I thank you for your kind attention. R.J Cook December 4th 2020
Summary of case involving Roberta Jane Cook
In 2016, I made an appointment at my local surgery with Dr Baines Clark, of Norden House Surgery, reference the possibility of me being transgendered. That surgery is Norden House Avenue Road Winslow, Bucks MK18. She referred me to Dr C.R Ramsay, a consultant pyschiatrist at Aylesbury’s Whiteleaf Centre. specialising in geriatric mental health care. He confrmed that I was in good physical and mental health – I have his report from 2016 confirming that I am suffering from no known mental illness . Ramsay concluded that I was a suitable candidate for the GIC and their services.
I then attended the GIC Clinic, had various assessments and consultations, but when it came to medication there were.several communications made known to me where Dr Roger Dickson of Norden House raised questions about my mental health and told them that my alleged heavy drinking meant my liver would struggle with hormone treatment. I was copied in to Dickson’s correspondence by Leighton Seal of the GIC who thanked Dickson for ‘five interesting letters.’
Dickson’s surgery had also ignored my prostate concerns since 2003 and my seriously raised free testosterone and abnormal Sex Hormone Binding Globulin ( SHBG ) levels on the basis that this was probabaly linked to alcohol abuse. By the way, I am not a heavy drinker and spent years working as an HGV driver until lockdown.).’This correspondence, from Dickson to Leighton Sea,l came one year after I had changed my name and conformed to their dress and behaviour requirements. I was offered no explanation or evidence.
As a matter of fact, taking anti androgens and alcohol is a serious health risk, so if I was a ‘drinker’ they were negligent at the GIC or suspected Dickson of lying. I am hypothyroid so regular liver and kidney function blood checks were routine for me. Dickson and his colleagues had regfularly signed me off on medicals as fit to drive HGVs, noting that I was not an alcoholic or mentally ill.
Dr Leighton Seal of the GIC overruled Norden House. Hormones, anti androgens and injections effectively chemically castrating me were prescribed. By February 2018, I was overdue to be listed for GRS ( Gender Reassignment Surgery ).
So, at my February 2018 meeting with Dr Kirpal Sahota of the GIC , Dr Sahota announced, apparently out of the blue, that my GRS was conditional on me taking anti psychotic drugs. She also said that I needed sessions with a psychiatrist from the Whiteleaf Centre. She had a male colleague present with a view to my long term therapy under this dangerous medication. Had the GIC et al done their job properly, and this not being connected with Norden House misconduct, then this medication with reasons would have been mentioned to me at the beginning – not after high risk hormone and anti androgen treatment. As it was, hormones, anti androgens, injections, facial hair removal and conforming to their dress code, my identity had been overwhelmed and myself put at risk from hate crime and social ostracism. In this context, I was suddenly expected to take anti psychotics, function and survive.
The situation is now compounded by Covid 19 lockdown, my son and I facing homelessness because of what has been done to me. One does not have to be mad to commit suicide – they know that. My ex wife admitted her habit of hitting me, and there was much worse, leading me to attempt hanging from a door handle in March 2007. You need to know this as my medical records appear to be subject to edit and direction. My ex wife was a senior employee of Dr Roger Dickson & Co – my GP practice. I also spent several years working there as a handyman, attending their social functions. My work there included extending the staff car park using a large digger, plumbing and re roofing an outbuilding.
As a psychology post grad, I had knowledge of anti psychotics, how they work, purpose and side effects. I was simply told that they would make me better without being told why they suddenly thought I was seriously mentally ill. Offering a path to over due GRS, Dr Sahota’s words were. ‘We would like you to take the medication, it will make you feel better and then we can deal with the GRS. Is that a deal ?’ I said no, also refusing the group therapy sessions and Whiteleaf psychiatric consultations. By this time my body was physically altered, along with hormone effects on my mental state. My genitals have since wasted away to the point where GRS would be very difficult if at all possible to any good worth while effect. Still Norden House, Whiteleaf and the GIC refuse to explain anything relating to me and gender reassignement..
The same month in 2018, prior to Ramsay’s visits., Sahota wrote to my GP, copying me in to a letter she had sent to my GP, informing him that I had secure female identity and was keen to proceed fo GRS. The letter approved further castration injections with the purpose of reducing my testosterone level to the approved level for surgery. Curiously, a few days later, psychiatrist, Dr C.R Ramsay arrived unannouced, along with a medical student and mental health nurse. I had just returned from a 13 hour HGV – which Ramsay turned into alcoholism, along with calling my efforts to defend myself ‘pressured speech’ which was a sign of a paranoid personality disorder – his ultimate and damning diagnosis..
I was warned that hospital was a possibility, so would best invite them in if I wanted a chance to avoid that. Two further afternnon sessions followed, both times after I had been at work – my usual work start times were between 0100 and 0200 hours. This is relevant because it was my custom to sip a glass of wine after work and prior to bed before my next shift
I protested against Ramsay’s intrusions.
After my third consultation, and well over a month later Ramsay phoned to ask me if I would accept a second opinion because GIC ‘wanted something stronger’ than he had written about me. I was working at the time, but he persisted. I told him that it was up to him to make that decision. I later discovered that Ramsay had already informed the GIC that I had refused a second opinion before he even asked me. Ramsay concluded that I have abnormal psychology as well as paranoia and recommended a multi agency approach to monitoring me, but ‘hospital is not needed yet;’ He also concluded that I am anti social, secretive and cannot relate to others or sustain relationships. That was 2 years ago.
Neither Norden House. Whiteleaf or GIC have so far responded to the questions raised here. Obviously I have thought of suicide in this impossible situation. Paranoia is ‘abnormal suspicion’, schizophrenia is normally taken as multiple personality. I have had no empirically based explanation as to why they suggest all of this applies to me, and if it does then why were these agencies so careless and incompetent as to not notice before February 2018 and when GRS should have been imminent. If they had this view before then, why not act and why not eplain themselves to myself or my son ?
Several months ago Dr Kimble, of Norden House, wrote informing me that he had written to ask the GIC for an update on my status with them. I wrote thanking him, noting it would be interesting as to their reply, regarding what they did or didn’t say. Not surprsingly, I have not been told anything. .
So, in conclusion, if there is any truth in allegations and mental health diagnoses , then the key question is why on earth was I ever recommended for such serious gender re assignment treatment, lasting for 2 years, what were the reasons, the details of diagnosis etc ?. If they do not stick by their allegations and diagnosis, why not because it obviously implicates them in misconduct and misdiagnosis otherwise ? They were asking me at the GIC to take take very dangerous anti psychotics. as part of a bargain for sex change surgery ? That is serious, demanding serious explanation, the details should be provided on paper, also explaining all parties involved and why it took so long. They have refused to do that by ignoring all of my requests.
So the situation pertains and worsens. The effect on my physical and mental health has been extreme, my alarm and distress is ongoing – worsening in fact. The physical and psychologcal damage is dreadful and on going. leaving me in gender limbo, impotent and infertile. There is clear evidence of prejudice, malpractice, medical neglect, questionable diagnosis and practice – with external influence and malice that needs to be verified and explained to me in writing..I can answer any questions arising from what the various involved parties may offer in their defence. All concerned have had ample opportunity to explain themselves to me. I think their silence says a lot about them.
Yours Sincerely R.J Cook


It is a hate crime to suggest that girls are being forced toward uncomfortablle old fashioned male type behaviour while sis males are driven in the other direction, growing up in once parent families with traditional male role models O.K for girls but not boys – all in the name of equalityy ( sic ) R.J Cook.
Trends in suicide death risk in transgender people: results from the Amsterdam Cohort of Gender Dysphoria study (1972–2017)
C. M. WiepjesM. den HeijerM. A. BremmerN. M. NotaC. J. M. de BlokB. J. G. CoumouT. D. Steensma First published: 18 February 2020 https://doi.org/10.1111/acps.13164Citations: 2SectionsPDFToolsShare
Abstract
Objective
This study explored the overall suicide death rate, the incidence over time, and the stage in transition where suicide deaths were observed in transgender people.
Methods
A chart study, including all 8263 referrals to our clinic since 1972. Information on death occurrence, time, and cause of death was obtained from multiple sources.
Results
Out of 5107 trans women (median age at first visit 28 years, median follow‐up time 10 years) and 3156 trans men (median age at first visit 20 years, median follow‐up time 5 years), 41 trans women and 8 trans men died by suicide. In trans women, suicide deaths decreased over time, while it did not change in trans men. Of all suicide deaths, 14 people were no longer in treatment, 35 were in treatment in the previous two years. The mean number of suicides in the years 2013–2017 was higher in the trans population compared with the Dutch population.
Conclusions
We observed no increase in suicide death risk over time and even a decrease in suicide death risk in trans women. However, the suicide risk in transgender people is higher than in the general population and seems to occur during every stage of transitioning. It is important to have specific attention for suicide risk in the counseling of this population and in providing suicide prevention programs.
Significant outcomes
- Suicide death risk in trans people did not increase over time.
- Suicide deaths occurred during every stage of transitioning.
- Suicide death risk is higher in trans people than in the general population.
Limitations
- Psychological comorbidity was not known.
- No data were available for people on the waiting list for their first appointment.
Introduction
Gender dysphoria (GD) refers to the distress related to a marked incongruence between one’s assigned gender at birth and the experienced gender (1. Trans people are diverse in the intensity of experienced GD (2, their needs for medical transition (3, and the impairment that GD can have on their life. Studies focusing on the wellbeing of trans people show a greater vulnerability for experiencing mental health problems compared with the non‐trans (cis) population (4. Most prevalent are affective and anxiety problems (5–7, often accompanied by feelings, thoughts, or behaviours linked to suicidality (8, 9.
The prevalence of suicidality in trans people in suicidal ideation, suicidal attempts, and suicide death rates is studied in varying degrees and shows high variability in findings. A systematic review by McNeil et al (9. reported suicidal ideation rates across 17 identified studies, ranging from 37% (10 up to 83% (11. Prevalence rates on suicidal attempts in trans people, which are generally observed to be lower than suicidal ideation, showed to be lower but also with a wide variation in reported rates, ranging from 9.8% (12 up to 44% (13. Since structured prevalence studies on suicide deaths are lacking in the transgender literature, an estimation comes from a limited number of studies reporting on suicide death rates in small study samples. Derived from a systematic review on suicidality in trans people by Marshall et al. (8, suicide death rates varied from 0% (14 to 4.2% in a sample of 24 post‐treatment trans people from Sweden (15. Six of these studies only included postsurgical people (14–19, whereas two studies also included trans people who were only using hormones without surgery (20, 21. However, studies differentiating the treatment stage during which death by suicide occurred are lacking. In addition, studies differentiating between suicide in trans women and trans men are scarce. While some studies found that trans men have a higher risk of suicide attempts than trans women (22, 23, other studies reported no differences in suicide attempts between trans women and trans men (24, 25. Only one cohort distinguished suicide death risk in trans women and trans men and found that trans women had an increased risk of suicide death compared with trans men (20, 21.
Aims of the study
The aim of the current study is to explore the overall suicide death rate in trans women and trans men in the largest clinical cohort of gender‐referred people seen at the Center of Expertise on Gender Dysphoria of the Amsterdam University Medical Centers between 1972 and 2017 the Netherlands (26. In addition, the change in incidence of suicide death rate over time and at what stage in transition (pretreatment, during hormonal treatment and/or surgical phase, or post‐treatment) suicide deaths were observed was explored. The relevance of such information is to get a greater understanding of how large the risk is in clinically referred transgender people and whether suicide prevention interventions should focus on specific stages in transition or not.
Material and methods
Study design
A retrospective chart study was performed, including all people who once visited the Center of Expertise on Gender Dysphoria of the Amsterdam UMC, Vrije Universiteit Amsterdam, the Netherlands, between 1972 and 2017. The selection of the study population is described previously (26. A total of 8263 adults, adolescents, and children were included, with a median age at first visit of 25 years (range 4 to 81 years) and a median follow‐up time of 7.5 years (range 0.0 to 45.5 years). Information on death occurrence, time, and cause of death was obtained by cross‐checking multiple sources: the National Civil Record Registry (21, which contains date of birth and date of death of all inhabitants of the Netherlands, and the hospital registration system, medical, and psychological files for cause of death.
The Medical Ethics Review Committee of the Amsterdam UMC, Vrije Universiteit Amsterdam, reviewed this study and determined that the Medical Research Involving Human Subjects Act (WMO) did not apply to this study. Therefore, and because of the retrospective design, necessity for informed consent was waived.
Treatment
After an initial visit to the endocrinologist (for adults) or child psychiatrist (for children and adolescents), all people were referred to the psychology department for the diagnostic phase. In this phase, people were seen to gain insight into their experienced gender identity, to verify whether they fulfill the diagnosis gender dysphoria, to explore their treatment desires, and to prepare them for possible medical interventions. After this phase, people may start with hormonal treatment. Trans women received treatment with anti‐androgens and estrogens. Trans men were treated with testosterone. In adolescents, treatment first started with a period of puberty suppression, followed by estrogens of testosterone around the age of 16 years (27.
Surgical interventions can be offered to people aged 18 years or older. Depending on the desired treatment, the surgery is preceded after at least one year of hormonal treatment (genital surgery) or can be offered after the diagnostic phase (e.g., breast removal). After surgery, all people were usually seen every 2 years for medical check‐up.
Statistical analyses
Characteristics of the population were shown as median with range due to the non‐normal distribution. The total number of people seen at our center and the total number of suicide deaths were counted and were expressed as percentages as well as incidence per 100 000 person years. For each year, the number of people at risk and the number of people who died by suicide were calculated. Cox regression analyses were performed to calculate hazard ratios (HR) with corresponding 95% confidence intervals (95% CI). Date of first visit was used as start date of follow‐up. The end date of follow‐up was either date of death or date of closing the database (December 31, 2017). Suicide death was analyzed as event. To analyze whether the incidence of suicide deaths changed over time, the year of first visit was added as determinant to the analyses. Analyses were adjusted for age at first visit as age might be related to suicide death risk. Time between date of suicide death and first visit, and between date of suicide death and start of hormonal treatment, if applicable, were calculated. All analyses were performed for the total population and were stratified for trans women and trans men.
All analyses were performed using STATA Statistical software (Statacorp, College Station, TX, USA), version 15.1.
Results
The characteristics of the study population are shown in Table 1. In total, 8263 people attended the gender identity clinic, of which 5107 were trans women (median age at first visit 28 years, range 4 to 81 years) and 3156 were trans men (median age at first visit 20 years, range 4 to 73 years). The median follow‐up time was 7.5 years (range 0.0–45.5 years), which was longer in trans women (10.2 years, range 0.0–45.5 years) than in trans men (4.8 years, range 0.0–45.5 years). The total follow‐up time was 92 227 person years (64 287 in trans women and 27 940 in trans men). Table 1. Characteristics of the study population (A) and the people who died by suicide (B)
| Total | Trans women | Trans men | |
|---|---|---|---|
| (A) | |||
| Number of people | 8263 | 5107 | 3156 |
| Age at first visit, year | 25 (4–81) | 28 (4–81) | 20 (4–73) |
| Follow‐up time, year | 7.5 (0.0–45.5) | 10.2 (0.0–45.5) | 4.8 (0.0–45.5) |
| (B) | |||
| Number of suicides | 49 (0.6%) | 41 (0.8%) | 8 (0.3%) |
| Age at first visit, year | 31 (15–59) | 31 (15–58) | 21 (16–59) |
| Age at time of suicide, year | 41 (18–66) | 41 (18–66) | 36 (21–60) |
| Follow‐up time, year | 6.7 (0.6–32.7) | 6.7 (0.6–32.7) | 6.7 (0.6–23.1) |
| Time between start hormones and suicide, year | 6.4 (0.4–32.5) n = 42 | 6.1 (0.4–32.5) n = 35 | 6.9 (3.7–23.1) n = 7 |
- Data are shown as number or median (range).
Forty‐nine people died by suicide: 41 trans women (0.8%) and 8 trans men (0.3%), which is 64 per 100 000 person years in trans women and 29 per 100 000 person years in trans men. The median follow‐up time between first visit and suicide death was 6.7 years (range 0.6 to 32.7 years) in trans women and 6.7 years (range 0.6 to 23.1 years) in trans men. Trans women had a higher overall suicide death risk than trans men (per year: HR 2.26, 95% CI 1.06–4.82). Four suicide deaths occurred in individuals who were referred to the clinic before the age of 18 (0.2%), which is a lower risk than in adults (0.7%, P = 0.010).
The course of number of people at risk and the number of people who died by suicide over the years is shown in Fig. 1. Overall suicide deaths did not increase over the years: HR per year 0.97 (95% CI 0.94–1.00). In trans women, suicide death rates decreased slightly over time (per year: HR 0.96, 95% CI 0.93–0.99), while it did not change in trans men (per year: HR 1.10, 95% CI 0.97–1.25). Adjustment for age at the first visit did not change these numbers.

As the median follow‐up time between first visit and suicide death was 6.7 years, subgroup analyses were performed in those who had their first visit before 2011. This did not change the outcomes: trans women (n = 3115) HR 0.94, 95% CI 0.91–0.98; trans men (n = 1269) HR 1.02, 95% CI 0.90–1.16).
Of the 49 people who died by suicide, 35 had a face‐to‐face contact with the endocrinologist or psychologist of the gender identity clinic in the previous two years, while the other 14 people were no longer in active counseling with the clinic. Sixteen of the 35 people who recently had visited the clinic, only came for a medical check‐up, as they were postsurgery (vaginoplasty or phalloplasty). Two people were in the surgery trajectory, and 17 were still in the diagnostic or hormonal phase at time of suicide. The transition phases separately for trans women and trans men who died by suicide are shown in Table 2. Table 2. The occurrence of suicide deaths distinguished for transition stage, and trans women or trans men
| Total (n = 49) | Trans women (n = 41) | Trans men (n = 8) | |
|---|---|---|---|
| In active counseling | 35 | 29 | 6 |
| In diagnostic or hormonal phase | 17 | 16 | 1 |
| In surgical phase | 2 | 0 | 2 |
| Only medical follow‐up care | 16 | 13 | 3 |
| No active counseling | 14 | 12 | 2 |
- Data are shown as number. In active counseling is defined as a face‐to‐face contact with the endocrinologist or psychologist of the gender identity clinic in the previous two years.
The mean number of suicides in the years 2013–2017 was higher in the trans population (40 per 100 000 person years; 43 per 100 000 trans women and 34 per 100 000 trans men) compared with the Dutch population in this time frame (11 per 100 000 person years; 15 per 100 00 registered men and 7 per 100 000 registered women) (28.
Discussion
The current study investigated the suicide death risk in the largest clinical cohort of gender‐referred individuals to the Center of Expertise on Gender Dysphoria at the Amsterdam UMC, the Netherlands, between 1972 and 2017. Findings from the chart reviews showed us a decrease in suicide death risk over time in trans women and no change in suicide death risk in trans men. Trans women, however, showed a higher suicide death risk than trans men. Between 2013 and 2017, the suicide risk in Dutch referred transgender people (40 per 100 000 person years) showed to be three to four times higher than the general Dutch population (11 per 100 000 person years) (28. Evaluation of transition stage in relation to suicide deaths showed that approximately two‐third of the observed suicides occurred in those who were still in active treatment (diagnostic, hormonal, or surgical phase). The incidence of suicide deaths and transition stage was similar in trans women and trans men.
Suicidal behaviour is a complex phenomenon that is a result of many individual (age, male sex assigned at birth, previous suicide attempts, mental health history, substance abuse) as well as more distant environmental factors. A recent literature review clearly demonstrates the specific risk factors for suicide in sexual minority youth, which includes negative social environments, inadequate support within the closest social network, and an absence of lesbian, gay, bisexual, and transgender (LGBT) movements in communities (29. In our cohort, both trans women and trans men show a three‐ to four‐fold elevated risk of suicide compared with the population rate in the Netherlands and can therefore be considered a high‐risk group. Although the Netherlands is known for its tolerance toward sexual minority groups in comparison to most countries in the world (30, the societal position of trans people is generally less favorable compared with the lesbian, gay, bisexual, and cis‐gender population. Furthermore, compared with trans men, the societal position of trans women is lower (31, 32.
In the Netherlands, between 1972 and 2017 suicide rates showed a fluctuating course. Our finding of a slightly decreasing suicide risk in Dutch trans women may confer some hope. Recent studies showed an increase in societal acceptance toward lesbian, gay, bisexual, and transgender people (31, and indications of an increase in social‐economic status over the years (33. Although specific information on trans men and trans women is unavailable, it is conceivable that the improvement of societal position may have effect on the psychological functioning and the prevention of suicidal risk in trans women. The cause of this increase in tolerance seems largely to be the effect of a national and international increase in visibility and attention for trans people in media and society. Another explanation may be that, with the increase in attention and acceptance, the threshold for transgender people to seek treatment or professional help has become lower over the years. This is also reflected by the increase in referrals each year (26. Lastly, with the increase of knowledge in this field and the literature about the vulnerability of the transgender population for suicidal ideation, suicidal attempts, and suicide death rates, it is conceivable to assume that the attention to these risks has increased in clinical counseling and may have its effect on prevention of suicide deaths over the years.
Although the incidence of suicide deaths in trans women decreased over the years, the overall incidence still showed to be higher in trans women compared with trans men. Conflicting results in literature are reported about the risk of suicide attempts between trans women and trans men. Some studies reported that trans men had a higher risk of suicide attempts than trans women (22, 23, while in other studies no differences in suicide attempts between trans women and trans men were found (24, 25. Only two studies looked at the differences in the risk of death by suicide between trans women and trans men and found that trans women had an increased risk compared with trans men (20, 21. However, these two studies were earlier studies performed in our center and therefore include a smaller part of our current study population.
An important finding was that the incidence for observed suicide deaths was almost equally distributed over the different stages of treatment. Although the distribution showed that one‐third of the suicides occurred in people who were no longer in active treatment in our center, the other two‐third of the people who died by suicide still visited our center in the previous two years. About half of these last two‐third people were still in active diagnostic or medical treatment, while the other half completed their transition and only came for a medical check‐up. This indicates that vulnerability for suicide occurs similarly in the different stages of transition. Although the literature on suicide risk factors is comprehensive, and particular suicidal risk factors like verbal victimization, physical and sexual violence, and the absence of social support (9, 34, may apply for transgender people in all stages of transitioning, it seems clinically highly relevant to understand and explore possible differences in motives and risk factors in the different stages of treatment. Therefore, future research on suicide deaths and suicide risk factors in transgender people should have a greater focus on transition status in relation to these motives and risk factors.
This study is performed in the largest cohort of gender‐referred people from the Netherlands, consisting of a large population of both adult and adolescent trans women and trans men at different stages of their transition with a long follow‐up time. However, this study has also some limitations. First, this study is a retrospective chart study. Although we used multiple strategies to obtain data about date of death, it is possible that we missed some data. Second, we did not have information about psychological comorbidities or other psychological information, such as social support. Third, we only had information about people who actually visited our gender identity clinic. Information about people on the waiting list for their first appointment was lacking.
To conclude, in our clinic we observed no increase in suicide death risk over time and even a decrease over time in suicide death risk in trans women was found. Since the suicide risk in the transgender population is higher than the general population and seems to occur during every stage of transitioning, it is important that (mental) health practitioners pay attention to this risk and create a safe environment in which these feelings can be discussed at all stages of treatment and counseling. Further research is necessary to investigate the motives behind the suicides, as input in the development of adequate suicide prevention programs.
Does Transition Reduce The Risk Of Suicide For Trans People?
by Richard Bayston — Last updated: 2020-08-14 in Emotional & Stress Management
Table of Contents
- Does Transition Reduce The Risk Of Suicide For Trans People?
- Does Transition “Work” For Trans People?
- Show full content
For transgender people medical transition is held up as the solution. Without it a high proportion of trans people will tragically eventually commit suicide. But how effective is it really at improving the quality of life of trans people?
Once doctors and the person in question are certain, beyond reasonable doubt, that a person is transgender, there are two treatment options. One involves trying to change the person — to make them not be transgender anymore. This option is widely discredited, is about as effective as it sounds, and should be avoided with the same scrupulousness as the “ex-gay” movement.
The other treatment option is usually medical transition.

Medical transition for a transgender person involves the use of hormone therapy to establish an endocrine environment appropriate to the target gender. Trans women will take a drug, usually spirolactone, to reduce the efficacy of the testosterone their testes are still producing. Other than that, hormone therapy for trans women is basically the pill; hormone therapy for trans men is basically steroids. That’s not intended to be belittling: testosterone is an anabolic steroid, and the birth control pill is a form of hormone treatment. Both of these hormones are naturally produced in the bodies of biological men and women.
If you’re a trans teen reading this and you’re thinking of self-medicating, be aware that the majority of adult trans people would warn you against this option, which can be dangerous or even fatal. By comparison, properly supervised medical transition for trans people can be comparatively safe and effective. The final step of medical transition involves surgical genital reconstruction to create genitals appropriate to the target gender. Trans men may have “top surgery” to remove the appearance of female breasts, while trans women can have an equivalent surgery to create breasts. Various genital construction surgeries, known colloquially as “bottom surgery”, also exist.
One powerful argument in favor of transition for trans people is the risk of suicide among transgender people. This is enormously high. Among trans people who can be easily “read” or “clocked” but haven’t transitioned, 42 percent will attempt suicide. Among trans people who suffer violence or mockery at school — and that’s most trans people of school age — 78 percent will attempt suicide. (Source: The Williams Institute/AFSP.) That’s more than three quarters. An Ottowa study found that 11 percent of transgender people in the Ottowa area attempted suicide in the single year of the study. (Source: Globe and Mail.) Deaths by suicide among trans people are equally shocking. In the USA, they occur at 800 per 100, 000 per year — 0.8 percent, compared to the whole-population level of 13 per hundred thousand.
Suicide attempts in the trans population occur at a rate almost 20 times the level for the whole population. Deaths by suicide occur at a rate 61 times the general population. (Sources: Globe and Mail, SpeakingofSuicide.com.)
With a problem that serious, it’s no wonder that transition is held up as a solution and referred to by trans writers as a lifesaver.
But does it live up to its reputation?
Ideally, to answer that question, we’d have a wealth of medical data. But unfortunately, that’s not the case. For one thing, getting hold of a properly designed study on the effects of transition isn’t easy because you can’t construct a double-blind controlled trial of transition the same way you can’t construct one for parachutes. It’s ethically impossible.
READ Myths About Transgender Identities
What evidence we do have appears ambivalent at first glance and appears to depend heavily on where the statement is coming from. Trans activists tend to say transition is effective, sharply reduces suicide risks, and saves lives. Anti-trans voices from the radical feminist and conservative camps will say that transition isn’t effective, causes more problems that it solves, and so on. Are these two camps arguing because there’s no real evidence?
Not really. In terms of the efficacy of transition in reducing depression, anxiety, and the risk of suicide among trans people, the conservatives are basically distorting the evidence for ideological reasons. It shouldn’t be any surprise to learn that trans people who transition still have higher anxiety and depression rates — and greater risk of suicide — than the general population. Even after transition, not all trans people “pass” as their target gender and many are carrying the legacy of years of stigma, shame, low incomes and dysmorphia. Unsurprisingly these factors all pay off in more anxiety and depression.
What we do see across the board is that transition is associated with reduced feelings of anxiety and depression, less suicidal ideation and better mental and physical health.
Lacking in Science December 6th 2020 – R.J Cook’s 70th Birthday
A Comment Much could be said about this above article. It raises key questions but doesn’t offer a creditable link between diagnosis, methodology, treatment or explain why gender reassignment is a solution to obvious and profound mental health / psychiatric conditions extant and rising in the wider populattion, not just those outing as transsexual.
There is a default rubbishing of conservative views – I don’t mean the vile bigotry and hate crimes of Trans Exclusionary Radical Feminists, I just mean those concerned about what appears to be more disruption to the natural world to accommodate a fantasy rainbow world that doesn’t face up to the common elements found in the backgrounds of so many aspiring transsexuals.
Their reasons or emotions here are more relevant to any statistic based solution than hormones, anti psychotics and surgery because there is no reason to suppose they will help a patient long term. Obviously, society must have a hidden agenda for the explosion of sex change cases, especially male to female.
There are significant issues just swept aside here, such as the prevalence of poor and poorly educated young people ( inevitably most from broken homes lacking male role models ) clutching at the perceived glamour and lower responsibilities of being female in a world of safe spaces – at a time when feminists viciously challenge what they call female stereotypes and would ban the transsexuals very existence if they could.
At the very best, this article seems to be saying that sex change ( sic ) by removing male biology is a possible cure for suicide but doesn’t always work.
If sucide is the key issue, how come the Tavistick Gender Identity Clinic, among others – working from the DSM -Diagnosis Statistics Medication – currently 6kg and ever expanding psychiatric babble bible – uses the DSM view that being transgendered is not a mental illness.
The world of psychiatry has always existed to explain away and justify how society’s powers, exploitation, lies, wars and greed drives people mad – by blaming the people. Radical psychiatrist R.D Laing, whose work I studied at university, called psychiatrists society’s prostitutes. I can’t judge all psychiatrists or prostitutes, but I think he has a point.
Suicide and depression are rising across the board. Offering sex change as a solution without better means of classification and diagnosis is asking for trouble. It is all the worse because so many never pass as the opposite sex. If the likes of Tavistock Clinic were compared to those selling cars they would face the wraith of Trading Standards. The DSM and Tavistock Gender Identity Clinic is hot on drugging people, but lacking in science.
R.J Cook